Texas Children’s surgeons perform a landmark procedure
Texas Children’s Hospital surgeons who pioneered an in-utero procedure that has improved outcomes for children with spina bifida and for their mothers performed the 100th surgery of its kind on June 30, 2021 at Texas Children’s Fetal Center.
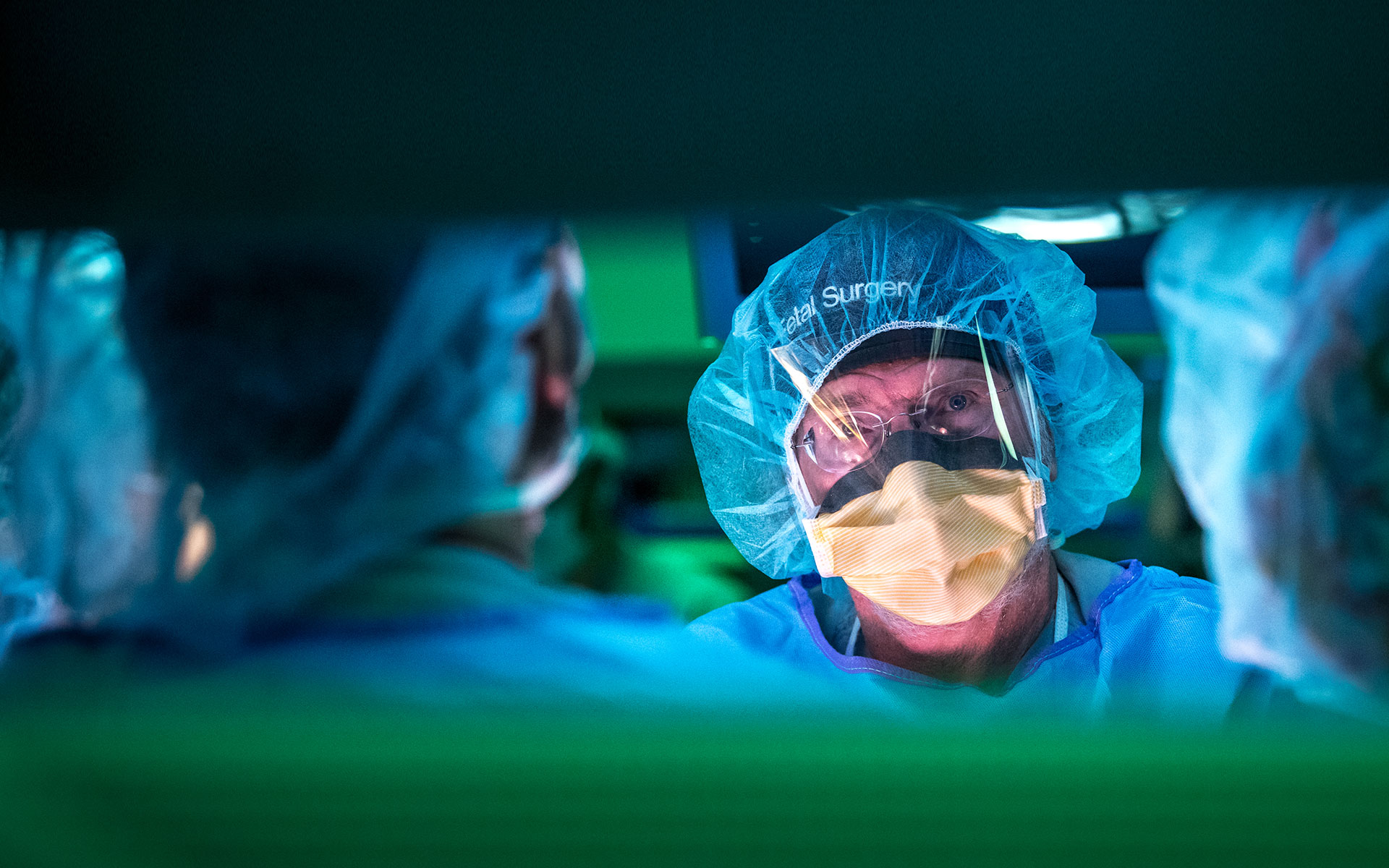
Dr. Michael Belfort, Obstetrician and Gynecologist-in-Chief at Texas Children’s Pavilion for Women, and Dr. William Whitehead, a pediatric neurosurgeon at Texas Children’s, performed the first successful two-port fetoscopic surgery for spina bifida in the world in 2014, using a technique they developed.
“This milestone was very exciting and had been years in the making at Texas Children’s,” said Belfort, who is also professor and chair of the Department of Obstetrics and Gynecology at Baylor College of Medicine. “Fetal surgery for spina bifida improves the baby’s chances of being able to walk and decreases the need for a shunt to drain fluid from the brain. Our procedure also gives the mother the chance of a normal term delivery and reduces her risk of the type of complications that may be seen with the open uterus approach. We hope that our outcomes will inspire other physicians to use this technique to improve spina bifida care across the world.”
About spina bifida
Spina bifida is the most common spinal defect in the U.S., affecting 1,500 to 2,000 babies born across the country each year. It occurs when the baby’s neural tube fails to close during the first month of pregnancy. Long-term effects can include difficulty in walking, abnormal bladder or bowel function, and the need for complex care for hydrocephalus — a buildup of fluid in the brain — which often requires the placement of a shunt from the brain to the abdominal cavity for drainage.
Surgeons at many hospitals around the world treat spina bifida prenatally, but most offer what is known as the “open procedure,” an operation in which the baby’s spine is repaired via a 7-10 cm opening in the uterus. This procedure, called a hysterotomy, increases the risk of pregnancy complications. Patients generally require a preterm (usually 34-35 weeks) cesarean delivery for the pregnancy, as well as all future pregnancies, to avoid the risk of uterine rupture. The babies may experience serious complications associated with premature birth. What Belfort and Whitehead developed is a minimally invasive fetoscopic method that offers the same neurological benefits for the child as the open method but presents less risk of complication for the mother and less risk of prematurity for the baby.
Advantages of our innovative approach
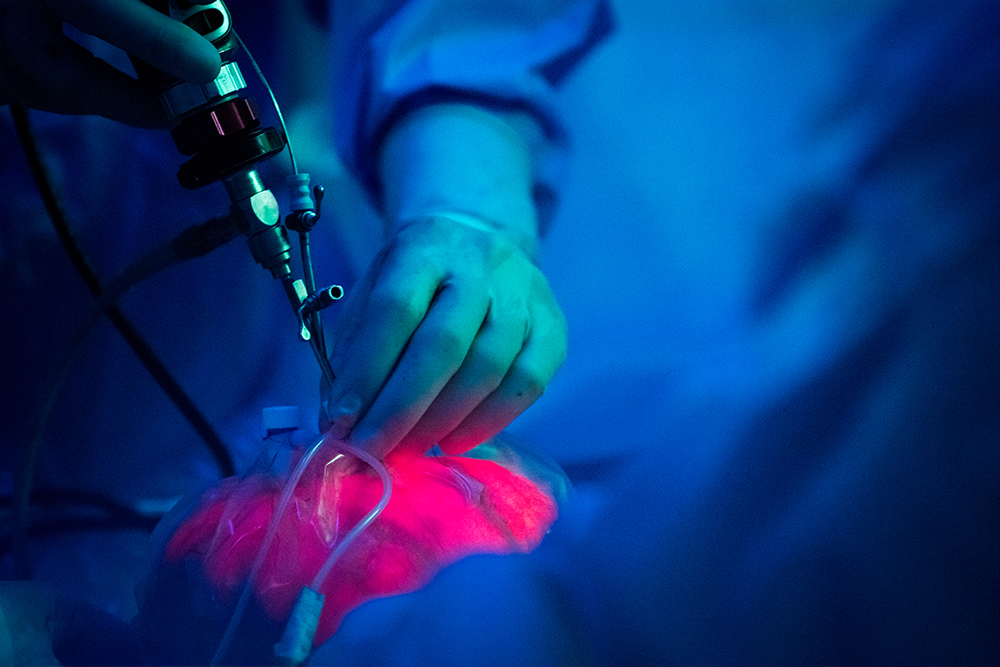
“In the two-port fetoscopic procedure we developed here at the Fetal Center, we externalize the uterus and place two 4 mm uterine ports into the amniotic cavity through which we operate,” Belfort said. “Throughout the course of the surgery, we remove most of the amniotic fluid and fill the uterus with carbon dioxide gas, which allows us to visualize the baby via a small camera inserted through one of the ports. The result is that most mothers have delivered around 38 weeks instead of at 34 to 35 weeks, and about 50% have had a vaginal delivery. They can be treated as any other pregnant woman would be.”
Belfort and Whitehead perform the surgery through two ports because they believe it is critical to use the lowest number of uterine incisions possible for the surgery to be successful and to minimize the chance that there will be rupture of the membranes and leakage of amniotic fluid after the surgery.
“The benefits to the mother are what convinced me to be part of this fetoscopic program, and I am even more pleased now to see that the later gestational age at birth also has benefits for the baby,” added Whitehead.
In 2011, Belfort and Whitehead began developing and practicing the two-port fetoscopic method, which they did for three years before they performed the procedure on their first patient. They collaborated with physicians in Barcelona, Spain to perfect the technique.
When first performed in 2014, the procedure was considered an investigational surgery, and the team began a research study that was overseen by four safety groups: the Institutional Review Board at Baylor College of Medicine, the U.S. Food and Drug Administration, a Data Safety Monitoring Board, and the Texas Children’s Hospital Fetal Therapy Board. Based on the positive outcomes seen and published, the procedure is now the standard of care for eligible patients at Texas Children’s Fetal Center.
Our commitment to the best possible outcomes
“Quality, safety and transparency are of the utmost importance to us,” Belfort said. “We don’t take these cases lightly, and we report all of our outcomes. We want patients to know that when they come here and put their life and their baby’s life in our hands, we take it very seriously.”
Belfort and Whitehead continue training physicians from all over the U.S. and the world to perform this novel procedure.
“There are babies on four continents and more than 12 countries who have benefited from this fetoscopic approach,” Belfort noted. “We hope to continue improving spina bifida outcomes for children and mothers, wherever they may be. Additionally, since fetoscopic surgery in a carbon dioxide gas environment now allows us to think of the uterus as a new surgical space, we are looking forward to innovating additional fetal surgeries to address other life-limiting or life-threatening congenital anomalies.”